Search
Presentation Details
| Association of structured preoperative cardiac risk algorithm completion with preoperative cardiac consultations, testing, and postoperative outcomes |
| Mandeep Kumar1,2, Kathryn Wilkinson2, Li Ya-Huei3, Rohit Masih1, Mehak Gandhi1, Julie Culmone1 1Hartford Healthcare Medical Group, Hartford, CT, United States 2University of Connecticut, Storrs, CT, United States 3Hartford Healthcare research program, Hartford, CT, United States |
BACKGROUND: Preoperative cardiac risk stratification algorithms are widely utilized in clinical practice. However, there is no standard approach for evaluating their impact. We studied structured algorithm completion via an electronic medical record (EMR) form and its impact requests for preoperative cardiology consultations, cardiac testing utilization and postoperative outcomes. METHODS: Retrospective cohort study comprising all elective surgical patients who underwent outpatient preoperative evaluation over a 2-year timeframe, dichotomized into two cohorts: July 1, 2021, to June 30, 2022 (pre-EMR form implementation) and July 1, 2022, to June 30, 2023, (post-EMR form implementation). Demographics, co-morbidities, resource utilization and receipt of surgical care were analyzed. Propensity score matching was used to adjust for differences. The primary outcomes were utilization of preoperative cardiology consultation, cardiac diagnostic testing, and 30-day postoperative major adverse cardiac events (MACE, composite measure of acute myocardial infarction (MI), cardiac revascularization, acute congestive heart failure (CHF), or all-cause mortality. Secondary outcomes were 30-day all-cause readmissions, emergency room visits and intensive care unit (ICU) utilization. RESULTS: 25,484 patients met inclusion criteria (mean [SD] age, 61.5 [15] years; 14216 [55.8%] female). Propensity score matching resulted in 11,654 well-matched pairs. Post-EMR matched cohort had lower cardiology consultation [Pre = 2698 (23.2%) vs. Post = 2088 (17.9%), p = <0.001] and echocardiogram [Pre = 808 (6.9%) vs Post = 591 (5.1%), p = <0.001] utilization. No statistically significant difference was noted in the 30-day postoperative outcomes, including MACE and secondary outcomes. In a sub-analysis performed in the post-EMR cohort, cardiology consultation is not associated with lower MACE risk. CONCLUSIONS: In this cohort study, consistent completion of the preoperative cardiac risk assessment algorithm via an EMR form was associated with lower cardiology consultation and testing utilization with no change in postoperative outcomes. This approach may be helpful in supporting guideline compliance for busy clinicians, reduce unnecessary resource utilization and have no adverse impact in outcomes, consistent with high value care. 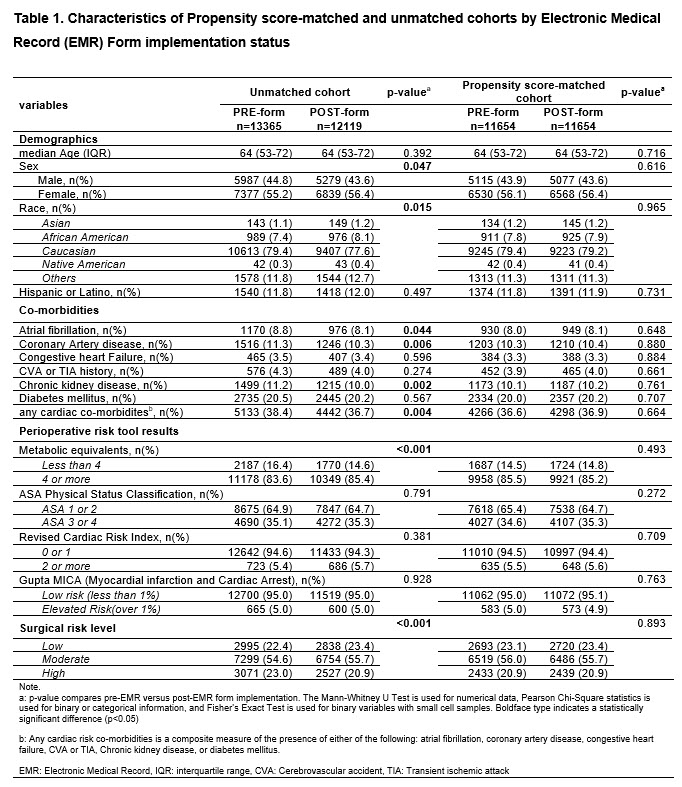 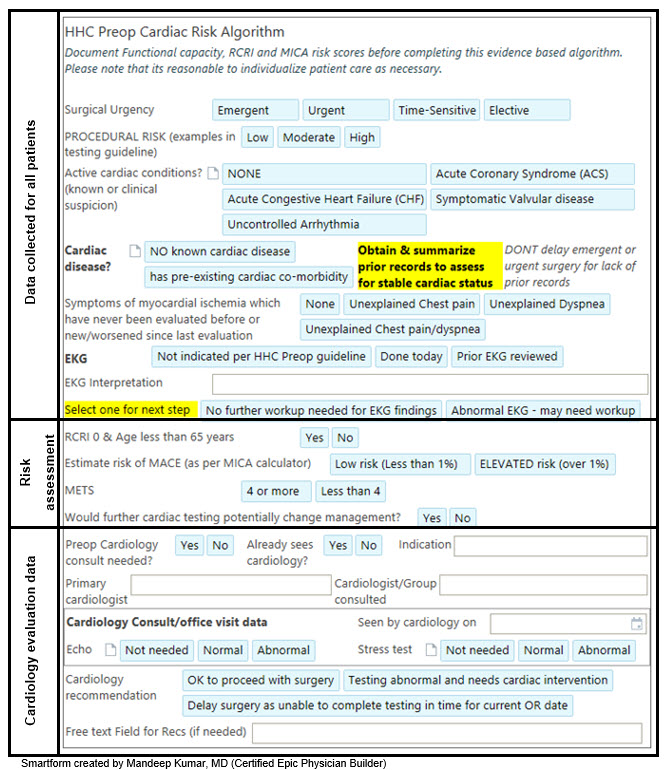 |