Search
Presentation Details
| Protocol to Identify Patients at Risk for Perioperative Myocardial Injury |
| Abhijai Singh, Kathryn Lauer, Christine Boxhorn, Stephanie Rossi, Abigail Thorgerson, Kurt Pfeifer, Barbara Slawski Medical college of Wisconsin, Milwaukee, WI, United States |
BACKGROUND: Several algorithms guide perioperative cardiovascular (CV) evaluation. High-quality studies regarding preoperative evaluation have since been published. We developed an updated evidence-based preoperative CV algorithm, implemented it as part of a clinical quality program, and examined outcomes in noncardiac surgery patients. METHODS: A preoperative algorithm was developed at a university-affiliated hospital to guide testing for asymptomatic patients at elevated risk for perioperative CV events. The algorithm combined practices from several guidelines and recent literature including risk calculation, use of the Duke Activity Status Index, and options to use NT-proBNP levels or stress testing in patients with major adverse cardiovascular event risks >1% (figure 1). Analysis compared the baseline (3/2017-2/2020) and post-implementation period 1 (“PI1,” Jan-Dec 2021, during which a NT-proBNP threshold of 300 pg/mL was used) and post-implementation period 2 (“PI2,” Jan-Aug 2022 with threshold of 200 pg/mL). Noncardiac surgery patients aged >18 seen in the preoperative clinic met inclusion criteria. RESULTS: The patient population in PI2 had more women and patients aged >65. Compared to baseline, more patients in PI1 and PI2 had NT-proBNP levels performed. Fewer had levels >200 pg/ml in PI2, but there was no difference when the threshold of >300 was used in PI1. Relatively few stress tests were performed in all periods, with no difference in results. Fewer patients had preoperative cardiology referrals in both PI2 and PI2. There was no difference in the rates of 30-day postoperative MI. Fewer post-implementation patients had troponin levels measured, but more had elevated troponin levels during their hospital stays. CONCLUSIONS: Introduction of an algorithm guiding preoperative evaluation to identify patients at risk for perioperative CV events increased the rate of NT-proBNP testing without changing stress testing rates. 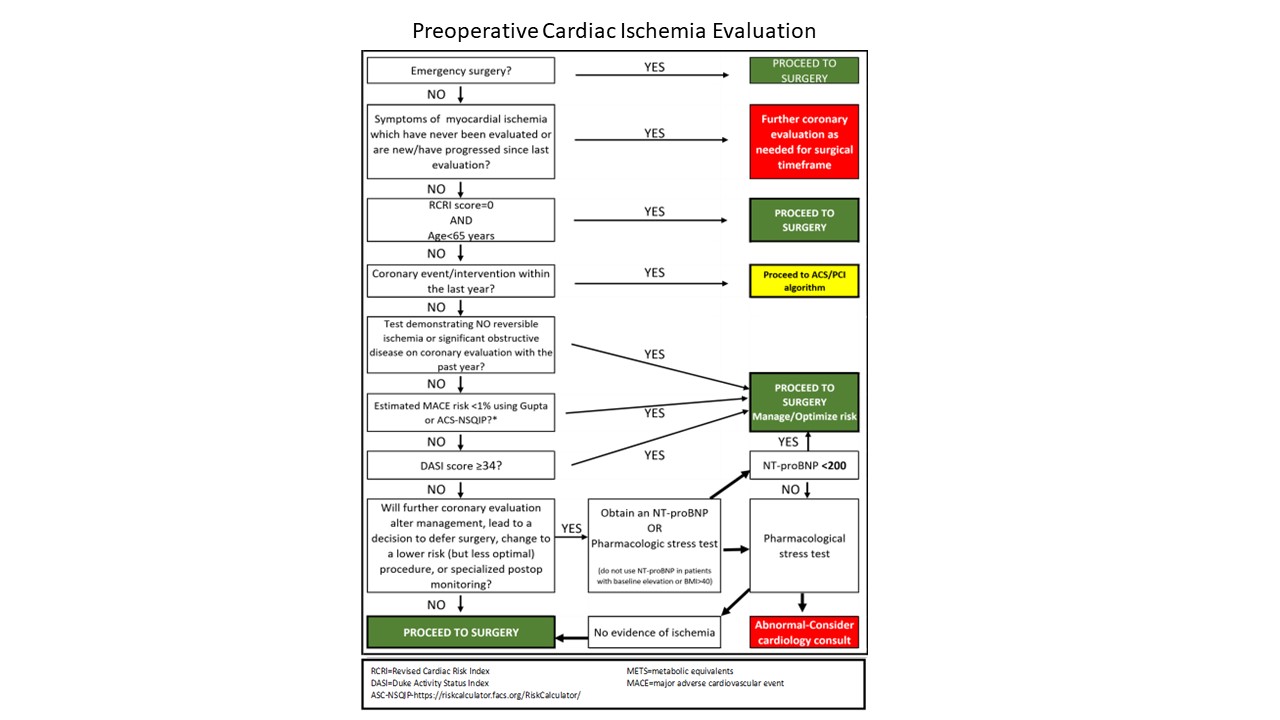 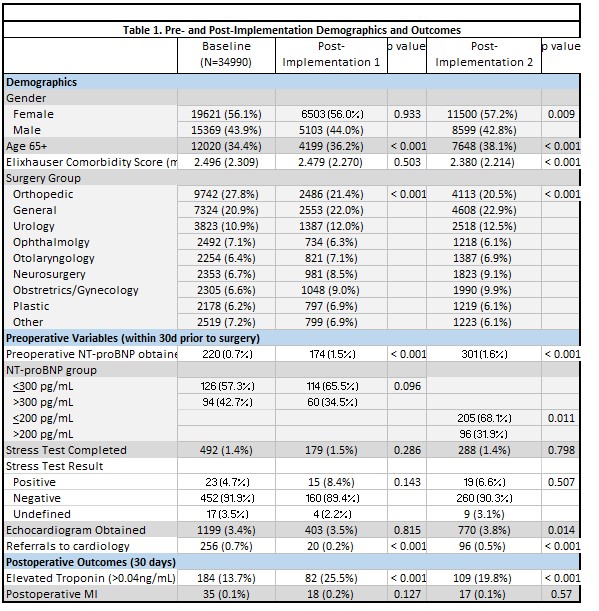 |